
Understanding Psoriasis: What Your Skin Might Be Telling You
It often starts with dry, itchy patches of skin—sometimes painful, always frustrating. For many, these flare-ups can feel embarrassing or isolating. But you’re not alone, and you’re definitely not powerless.
Psoriatic disease is a chronic skin condition that goes deeper than just surface-level symptoms. It’s linked to the immune system and often runs in families. Triggers can include stress, cold weather, skin injuries, certain medications, allergies, alcohol, and even a higher body fat percentage.
“Psoriatic disease is complex and often misunderstood,” says Vanessa Snow, Head of Medical Affairs at Johnson & Johnson Innovative Medicine. “We’re not just working on treatments—we want to help people recognise symptoms early and feel empowered to take action.”
What Does Psoriatic Disease Look Like?
This condition tends to come and go in cycles, with flare-ups lasting a few weeks or months before easing off. While there’s still a lot to learn—especially around the role of food—here are the five most common types:
Plaque psoriasis: The most common type. Think red, raised patches of skin covered in silvery-white scales, often found on the scalp, knees, elbows, or back.
Guttate psoriasis: More common in kids or young adults. Small red dots show up on the limbs or torso, usually after an illness like strep throat.
Pustular psoriasis: White bumps (filled with pus) surrounded by red skin, usually on the hands and feet.
Inverse psoriasis: Smooth red patches in skin folds, like under the breasts, armpits, or groin. Sweat and friction can make this worse.
Erythrodermic psoriasis: A rare but serious form that causes red, scaly skin across most of the body. It can be triggered by things like sunburn or certain medications, and often develops from unmanaged psoriasis.
Can It Be Treated?
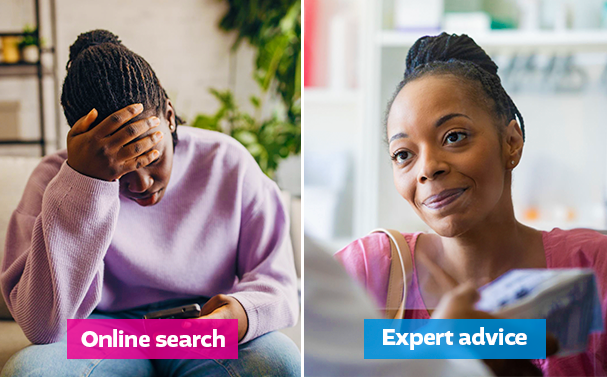
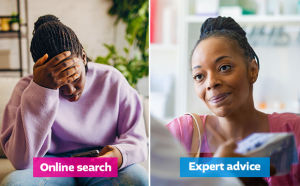
There’s no cure—yet—but there are ways to manage it. With the right care plan, you can reduce symptoms and take back control.
Here’s what might help:
See a doctor: This is your first and most important step. They might suggest moisturisers, vitamin D creams, or stronger options like steroid creams or coal tar. In more severe cases, medication that affects the immune system may be needed.
Consider light therapy: Exposing the skin to certain types of UV light (under medical supervision) can help.
Watch your weight: Research shows a strong link between obesity and psoriasis. A healthier lifestyle and diet could reduce flare-ups—and boost your overall wellbeing.
Act early: About 30% of people with psoriasis develop psoriatic arthritis, which affects the joints. That’s why an early diagnosis is so important.
Living With Psoriatic Disease
Managing this condition is a long-term commitment—but it doesn’t have to take over your life. Understanding your symptoms, finding the right treatments, and making a few lifestyle changes can make a big difference.
If you’re dealing with psoriatic disease, know this: you have options, support, and a way forward.















Post Comment